Displaying items by tag: intervention
Elevating Rural Mental Health Care
Growing up in rural Nevada on a cattle ranch, I am familiar with the benefits and downsides of rural living. I credit many of my core values as an adult to being raised in this environment. As I went through the process of becoming a psychologist, I began to realize the disconnect between the services available in urban areas, where I trained, and the services available to the community in which I was raised. The values I was taught as a child of equity and compassion have made it hard for me to see the disparities in what is available and what is actually accessible in mental health care.
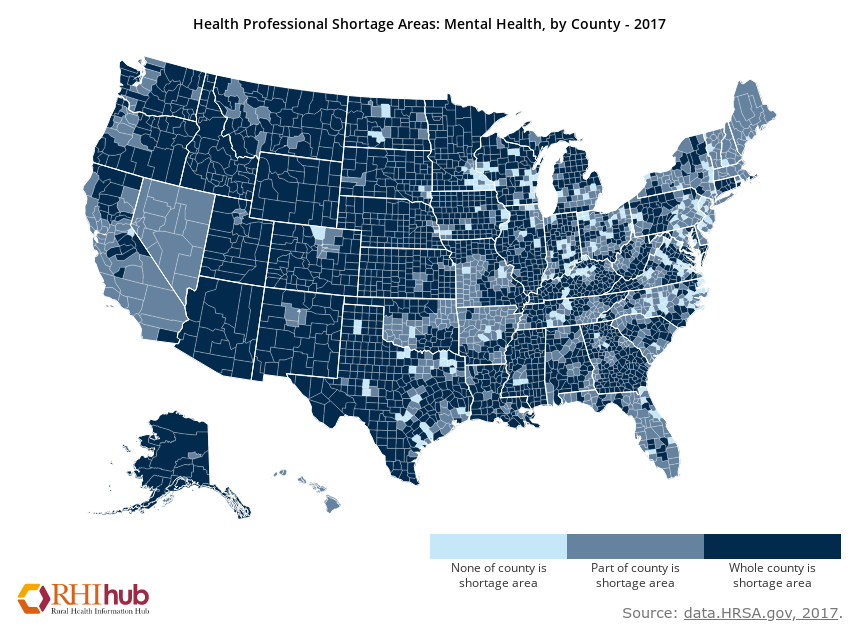
Access to mental health services is limited across our country. Those living in rural areas have an even harder time accessing health services. While rates of mental health concerns are similar in urban and rural areas (McCall-Hosenfeld, Mukherjee, & Lehman, 2014), the availability of mental health services in rural areas is significantly less. There are 39 psychologists for every 100,000 residents in urban areas, while only 16 for the same amount of residents in rural areas (Bolin, Bellamy, Ferdinand, Kash, & Helduser, 2015). Additional barriers are present for rural residents to seek mental health care. For example, they have further to travel, it takes more time/money/work leave to attend appointments, and it is more difficult to maintain confidentiality. For example, if your truck is parked in front of a building that says “Psychological Services” in a small town, your community may know that you are receiving services.
There are outreach efforts to increase awareness of identification and treatment options for mental health concerns, however, these efforts are not reaching the far corners of our country equally. This leaves rural residents with less information about signs of mental health concerns and available treatments. You know that healthy eating and physical activity are core components of weight loss. Do you know what to do if you have persistent fear or sadness? People in urban areas are more likely to know the answer than those in rural areas. If you have a physical health concern that you do not know how to address, you go to a doctor to get clarification and treatment. The same goes for mental health. However, the same values that make rural cultures beautiful and strong, can keep rural residents from reaching out for help when needed – independence, self-reliance, strong work ethic, putting others first, and close connections to the community.
Solutions have been proposed to address these concerns. These include integrating mental health providers into already established rural medical clinics, allowing patients to see both medical and mental health providers in the same location. Training rural teachers, religious leaders, bartenders, volunteer emergency staff, and other community members in the signs of mental health concerns and the how to respond appropriately and get community members connected with appropriate care. Incentives are offered for mental health providers that work in areas that are designated as mental health professional shortage areas as another way to increase access to care in rural areas.
One growing area is the provision of services through video-conferencing, or telemental health. This allows residents in rural areas to connect with providers that are geographically distant. Telemental health allows patients to meet with their provider from established medical and mental health clinics, their home, a library, their work, and parked in their car! As long as the patient is located in a private area, there are many options to connect with specialists in mental health care.
References & Resources:
ruralhealthinfo.org
Bolin JN, Bellamy G, Ferdinand AO, KashBA, HelduserJW. (Eds.) (2015). Rural Healthy People 2020.Vol. 1. College Station, Texas: The Texas A&M University School of Public Health, Southwest Rural Health Research Center. ISBN#978-1-4951-5242-9
McCall-Hosenfeld, J. S., Mukherjee, S., & Lehman, E. B. (2014). The prevalence and correlates of lifetime psychiatric disorders and trauma exposures in urban and rural settings: Results from the national comorbidity survey replication (NCS-R). PLoSONE,9(11).
https://doi.org/10.1371/journal.pone.0112416