Displaying items by tag: mental health
Presenter: Sarah Turley, PhD
Date & Time: September 19, 8:00 am to 9:45 am
Dr. Turley will discuss helpful navigation of power dynamics, relationship roles, sexual considerations and other dynamics unique to working with LGBTQ+ dyads as well as non-monogamous clients. She was the Director of Training for Psychology at the Salt Lake City VA Healthcare System, Senior Ethicist, and national faculty for VA Ethics on a national end-of-life initiative. Dr. Turley has a private practice and holds an academic appointment with University of Utah in Counseling Psychology teaching M.A. and Ph.D students.
Please note our meeting location: Meetings are conducted at the new Pride Center in Salt Lake City; 1380 S. Main St, Salt Lake City, UT 84115 (near the Bee’s Stadium) ‐ unless otherwise specified in the schedule. Parking is permitted anywhere in the parking lot. Enter the building through the main entrance, and turn right to find the conference room.
CEU’s have been approved for all in‐service programs by Utah Psychological Association. CEUs have been applied for from Utah NASW for all in-service programs and The Plan‐B Theatre Events . CEU’s are free for Guild members & $5 for non‐members, per meeting.
Jamie Lowe, a novelist and trauma survivor, is profiled this week on NPR’s This American Life. She lets people into her most vulnerable therapy moments while completing an Evidence Based Treatment for PTSD called Cognitive Processing Therapy. This powerful treatment is offered by expertly trained UCEBT clinicians. Contact us to find out more and learn whether this intervention may be a fit for you.
This American Life profiles Cognitive Processing Therapy for PTSD
Elevating Rural Mental Health Care
Growing up in rural Nevada on a cattle ranch, I am familiar with the benefits and downsides of rural living. I credit many of my core values as an adult to being raised in this environment. As I went through the process of becoming a psychologist, I began to realize the disconnect between the services available in urban areas, where I trained, and the services available to the community in which I was raised. The values I was taught as a child of equity and compassion have made it hard for me to see the disparities in what is available and what is actually accessible in mental health care.
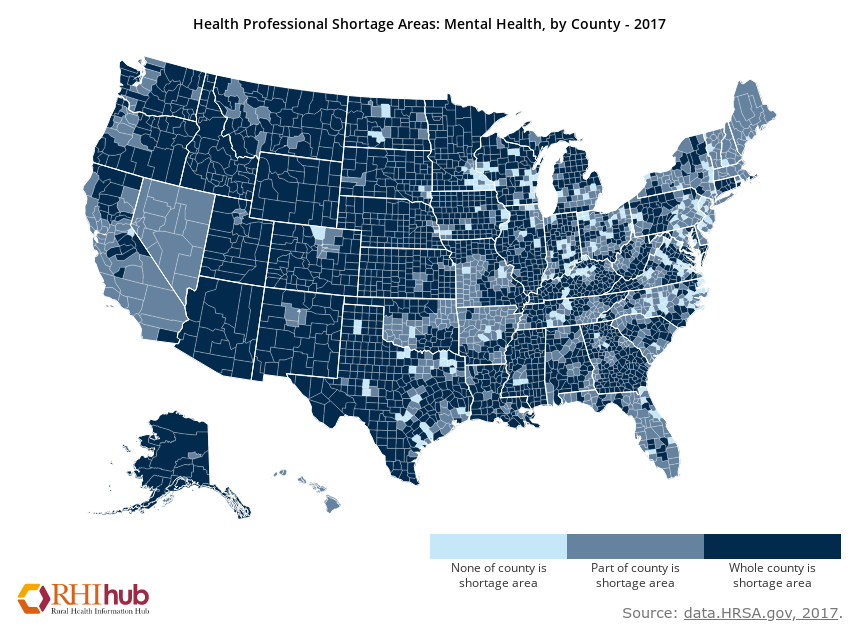
Access to mental health services is limited across our country. Those living in rural areas have an even harder time accessing health services. While rates of mental health concerns are similar in urban and rural areas (McCall-Hosenfeld, Mukherjee, & Lehman, 2014), the availability of mental health services in rural areas is significantly less. There are 39 psychologists for every 100,000 residents in urban areas, while only 16 for the same amount of residents in rural areas (Bolin, Bellamy, Ferdinand, Kash, & Helduser, 2015). Additional barriers are present for rural residents to seek mental health care. For example, they have further to travel, it takes more time/money/work leave to attend appointments, and it is more difficult to maintain confidentiality. For example, if your truck is parked in front of a building that says “Psychological Services” in a small town, your community may know that you are receiving services.
There are outreach efforts to increase awareness of identification and treatment options for mental health concerns, however, these efforts are not reaching the far corners of our country equally. This leaves rural residents with less information about signs of mental health concerns and available treatments. You know that healthy eating and physical activity are core components of weight loss. Do you know what to do if you have persistent fear or sadness? People in urban areas are more likely to know the answer than those in rural areas. If you have a physical health concern that you do not know how to address, you go to a doctor to get clarification and treatment. The same goes for mental health. However, the same values that make rural cultures beautiful and strong, can keep rural residents from reaching out for help when needed – independence, self-reliance, strong work ethic, putting others first, and close connections to the community.
Solutions have been proposed to address these concerns. These include integrating mental health providers into already established rural medical clinics, allowing patients to see both medical and mental health providers in the same location. Training rural teachers, religious leaders, bartenders, volunteer emergency staff, and other community members in the signs of mental health concerns and the how to respond appropriately and get community members connected with appropriate care. Incentives are offered for mental health providers that work in areas that are designated as mental health professional shortage areas as another way to increase access to care in rural areas.
One growing area is the provision of services through video-conferencing, or telemental health. This allows residents in rural areas to connect with providers that are geographically distant. Telemental health allows patients to meet with their provider from established medical and mental health clinics, their home, a library, their work, and parked in their car! As long as the patient is located in a private area, there are many options to connect with specialists in mental health care.
References & Resources:
ruralhealthinfo.org
Bolin JN, Bellamy G, Ferdinand AO, KashBA, HelduserJW. (Eds.) (2015). Rural Healthy People 2020.Vol. 1. College Station, Texas: The Texas A&M University School of Public Health, Southwest Rural Health Research Center. ISBN#978-1-4951-5242-9
McCall-Hosenfeld, J. S., Mukherjee, S., & Lehman, E. B. (2014). The prevalence and correlates of lifetime psychiatric disorders and trauma exposures in urban and rural settings: Results from the national comorbidity survey replication (NCS-R). PLoSONE,9(11).
https://doi.org/10.1371/journal.pone.0112416
DBT: Skills For Reducing Suicidal Distress
Zero Suicide Summit 7/19/2019
Dialectical Behavior Therapy: Skills For Reducing Suicidal Distress
By Sheila Crowell